Sunjay Kapur and Anaphylactic Shock – Lessons from a Tragedy
Understanding anaphylactic shock, recognising its lightning-fast onset, and acting decisively with epinephrine are the keys to turning a potential tragedy into a close call.
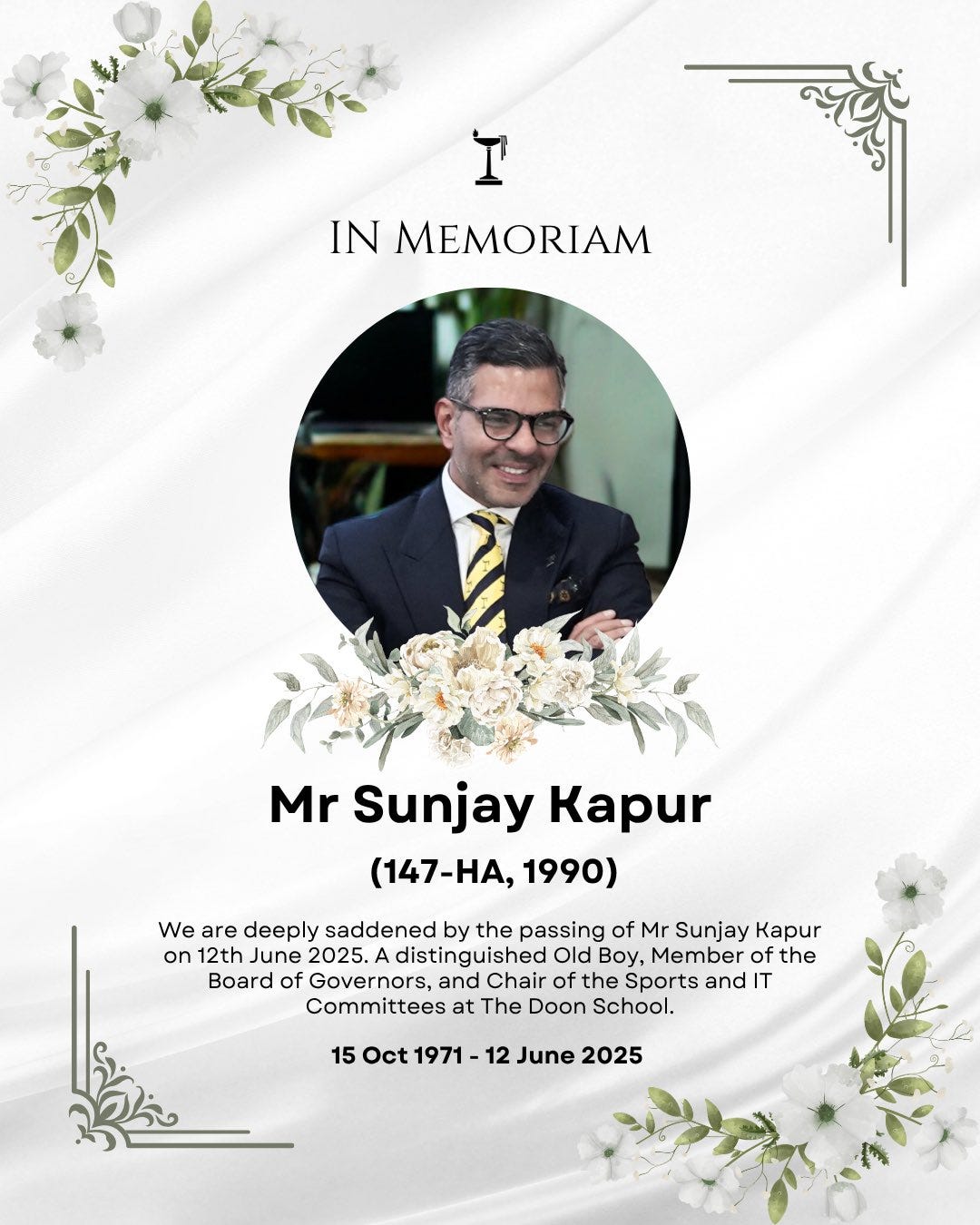
A High-Profile Tragedy Brings Anaphylactic Shock Into Public Focus
The untimely passing of industrialist and polo aficionado Sunjay Kapur on 12 June 2025, reportedly after swallowing a bee mid-match and suffering a fatal allergic reaction, has brought renewed public attention to anaphylactic shock—a swift, often unpredictable medical emergency. While the precise cause of death has not yet been conclusively established—as the official post-mortem report remains outside the public domain—reports circulating within the medical fraternity strongly suggest that anaphylaxis was the most likely trigger behind his sudden demise.
While Kapur’s name inevitably draws headlines, the purpose of this article is to explain the medical condition itself, offer practical guidance, and underscore the importance of awareness and preparedness, all in plain language and without medical jargon. As always, this article does not constitute professional medical advice.
(Disclaimer: this article is for general information only; we are not medical specialists.)
1. What Exactly Is Anaphylactic Shock?
Anaphylaxis is an extreme allergic reaction that sweeps through the body in minutes, releasing chemicals that dilate blood vessels, plunge blood pressure, and tighten airway muscles. When these circulatory changes are severe enough to starve vital organs of oxygen, the episode is labelled anaphylactic shock. Without rapid treatment, cardiac arrest can follow.
2. Why Can It Strike Anyone—Even Without Known Allergies?
First-time reactions are more common than many realise. A person may be sensitised by a silent earlier exposure (a bee sting months ago, trace peanut oil on cutlery, a dose of antibiotic) yet show no warning signs until the next encounter tips the immune system into overdrive. Roughly one in four severe reactions arise in people with no previous allergy diagnosis.
3. Typical Triggers
Insect venom – bees, wasps, hornets, fire ants
Foods – peanuts, tree nuts, shellfish, fish, milk, eggs, sesame, wheat
Medicines – penicillin-type antibiotics, NSAIDs, contrast dyes, some anaesthetics
Latex and certain chemicals
Exercise, alcohol, or extreme temperatures can amplify these triggers in susceptible individuals.
4. Warning Signs to Act On Immediately
Rapidly spreading rash or hives
Swelling of lips, tongue, or throat
Tight chest, wheeze, hoarse voice, repeated cough
Sudden dizziness, faintness, or “impending doom” sensation
Nausea, abdominal cramps, diarrhoea
Remember: skin changes can be absent in up to 20 % of cases—breathing difficulty alone can signal anaphylaxis.
5. First-Line Response: Epinephrine (Adrenaline)
If an auto-injector is available, use it without delay into the outer thigh, even through clothing (very short video):
Remove safety cap.
Press firmly against thigh until the click is heard or felt.
Hold for the suggested count (device-specific, usually 3–10 seconds).
Call emergency services straight after and lie the person flat with raised legs unless breathing is easier sitting up. A second dose may be given after 5–15 minutes if symptoms persist.
6. After the Ambulance: Monitoring & Biphasic Reactions
Symptoms can rebound hours later. Medical teams generally observe patients for at least four hours—and longer for severe cases—to guard against a biphasic episode.
7. Preventive Measures for At-Risk Individuals
Carry two auto-injectors at all times; devices expire after about a year.
Wear medical-alert jewellery.
Discuss venom-desensitisation or food allergy immunotherapy with an allergist if appropriate.
Read labels scrupulously; inform restaurants and friends of your allergy.
8. Sensible Precautions for Everyone
Even households without diagnosed allergies can lower risk:
Cover sweet drinks outdoors; use lidded bottles while cycling or playing field sports.
Avoid aggressive gestures toward bees; leave nests to professionals.
Dress in neutral colours, avoid strong floral perfumes when in gardens or orchards.
Learn the basics of auto-injector use—helping someone else might save a life.
9. Sport, Speed, and the “Open-Mouth” Hazard
Sports such as polo, cycling, or motor-racing increase the chance of insects hitting the face at speed. Mouthguards, visors, or simply keeping one’s mouth closed on fast runs can reduce that rare but catastrophic scenario that befell Sunjay Kapur.
10. Should Every Household Stock Epinephrine?
Not generally. An auto-injector is a prescription medicine best reserved for those with a documented risk or on a doctor’s advice. For most families, vigilance, basic first-aid knowledge, and prompt emergency calls remain the sensible standard.
11. Final Thoughts
Sunjay Kapur’s death was a heartbreaking reminder that life can pivot in a heartbeat—literally. Understanding anaphylactic shock, recognising its lightning-fast onset, and acting decisively with epinephrine are the keys to turning a potential tragedy into a close call. Share this knowledge widely, review your own readiness, and remember: in an emergency, seconds matter.